- Posts: 4388
- Thank you received: 94
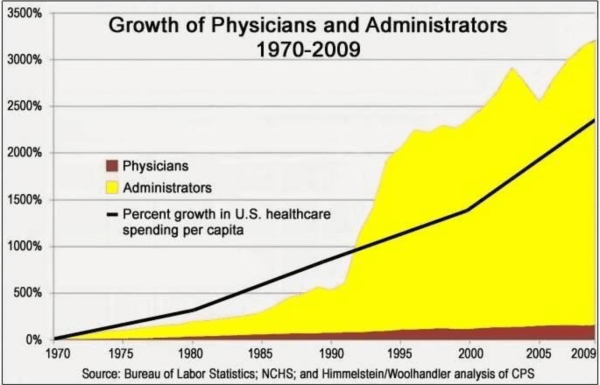
THE PROBLEM OF HEALTH CARE IN ONE GRAPH
- ramage
-
 Topic Author
Topic Author
- Mountain Legend
-

Less
More
11 Mar 2021 17:14 #1
by ramage
THE PROBLEM OF HEALTH CARE IN ONE GRAPH was created by ramage
Please Log in or Create an account to join the conversation.
- Rick
-

- Mountain Legend
-

Less
More
- Posts: 15594
- Thank you received: 163
11 Mar 2021 18:30 #2
by Rick
The left is angry because they are now being judged by the content of their character and not by the color of their skin.
Replied by Rick on topic THE PROBLEM OF HEALTH CARE IN ONE GRAPH
Exactly what's wrong with our government and all the agencies that make up our bloated bureaucracy. This is how government creates jobs.. layers and layers of non-essential people multiplying like rabbits.
The left is angry because they are now being judged by the content of their character and not by the color of their skin.
Please Log in or Create an account to join the conversation.
- FredHayek
-
- Mountain Legend
-

Less
More
- Posts: 30759
- Thank you received: 179
11 Mar 2021 21:56 #3
by FredHayek
Thomas Sowell: There are no solutions, just trade-offs.
Replied by FredHayek on topic THE PROBLEM OF HEALTH CARE IN ONE GRAPH
Agree, schools have the same issues.
Thomas Sowell: There are no solutions, just trade-offs.
Please Log in or Create an account to join the conversation.
- Pony Soldier
-
- User is blocked
-

Less
More
- Posts: 4749
- Thank you received: 43
12 Mar 2021 06:24 #4
by Pony Soldier
Replied by Pony Soldier on topic THE PROBLEM OF HEALTH CARE IN ONE GRAPH
So what happened in 1992 that caused that drastic change?
Please Log in or Create an account to join the conversation.
- homeagain
-

- Mountain Legend
-

Less
More
- Posts: 12795
- Thank you received: 173
12 Mar 2021 06:57 #5
by homeagain
ELECTRONIC RECORDS began to take hold (earlier) and then became the standard.
www.elationhealth.com/clinical-ehr-blog/history-ehrs/
Replied by homeagain on topic THE PROBLEM OF HEALTH CARE IN ONE GRAPH
Pony Soldier wrote: So what happened in 1992 that caused that drastic change?
ELECTRONIC RECORDS began to take hold (earlier) and then became the standard.
www.elationhealth.com/clinical-ehr-blog/history-ehrs/
Please Log in or Create an account to join the conversation.
- ramage
-
 Topic Author
Topic Author
- Mountain Legend
-

Less
More
- Posts: 4388
- Thank you received: 94
12 Mar 2021 07:48 #6
by ramage
Replied by ramage on topic THE PROBLEM OF HEALTH CARE IN ONE GRAPH
www.researchgate.net/publication/2866561...l_and_cultural_story
Abstract:
In 1983, DRGs became the price-setting system for the Medicare program in the United States. Why did the United States choose DRGs? The idea of setting 518 diagnostic payment rates for 4,800 hospitals seemed unimaginably complicated, too technical and an exercise in formula-driven cost control to some observers – an ambitious endeavor unlikely to succeed. Nevertheless, since its inception, the DRG system has been called the single most significant post-war innovation in medical financing in the history of the United States (Mayes 2006), and may be the most influential health care management research project ever developed. As the chapters in this volume attest, worldwide adoption of DRGs followed in the wake of this American experiment. Other competing patient classification systems could have been selected (Pettingill and Vertrees 1982). The range of policy options included flat rates per discharge, capitation, expenditure caps, negotiated rates, and competitive bidding (Smith 1992). Although researchers continue to experiment with alternative patient classification systems, a critical mass has formed around DRGs as the dominant design for measuring a hospital's casemix. A dominant policy design not only obtains legitimacy from the relevant community, future innovations must adhere to its basic features (Utterback 1996). A dominant design does not have to outperform other innovations; it merely has to balance the stakeholder interests. Though the control of rising health costs is a major policy issue, American hospitals had come to expect “pass-throughs, bail-outs, and hold-harmless clauses” from the political system (Smith 1992, p 44). © Cambridge University Press 2008 and Cambridge University Press, 2010.
DRG's started the movement to the paperwork world. In 1992, came the PPO's:
A definition from Wikipedia,
In health insurance in the United States, a preferred provider organization (PPO), sometimes referred to as a participating provider organization or preferred provider option, is a managed care organization of medical doctors, hospitals, and other health care providers who have agreed with an insurer or a third-party administrator to provide health care at reduced rates to the top insurer's or administrator's clients.
During the time leading to 1992, doctors and hospitials were scrambling to form alliances. Again several layers of administration were added to deal with the complexity. of these relationships.
In the Wikipedia article, it is noted that the first PPO started in St. Luke's Medical Center (now Presbytarian/St. Luke's) in 1990.
Then there was this: from the Orlando Sentinel Jan 1, 1992:
The most far-ranging change in Medicare since it began setting hospital rates in 1983 takes effect today. This time, Medicare is setting rates for doctors.
And also this: in the 80's, the merging of hospitals created such behemoths as Humana, HealthOne, United Healthcare, etc. The more complex the organization, the more administrators needed..
These factors and others became out of control in the early 1990s and it became "Katie bar the door".
Abstract:
In 1983, DRGs became the price-setting system for the Medicare program in the United States. Why did the United States choose DRGs? The idea of setting 518 diagnostic payment rates for 4,800 hospitals seemed unimaginably complicated, too technical and an exercise in formula-driven cost control to some observers – an ambitious endeavor unlikely to succeed. Nevertheless, since its inception, the DRG system has been called the single most significant post-war innovation in medical financing in the history of the United States (Mayes 2006), and may be the most influential health care management research project ever developed. As the chapters in this volume attest, worldwide adoption of DRGs followed in the wake of this American experiment. Other competing patient classification systems could have been selected (Pettingill and Vertrees 1982). The range of policy options included flat rates per discharge, capitation, expenditure caps, negotiated rates, and competitive bidding (Smith 1992). Although researchers continue to experiment with alternative patient classification systems, a critical mass has formed around DRGs as the dominant design for measuring a hospital's casemix. A dominant policy design not only obtains legitimacy from the relevant community, future innovations must adhere to its basic features (Utterback 1996). A dominant design does not have to outperform other innovations; it merely has to balance the stakeholder interests. Though the control of rising health costs is a major policy issue, American hospitals had come to expect “pass-throughs, bail-outs, and hold-harmless clauses” from the political system (Smith 1992, p 44). © Cambridge University Press 2008 and Cambridge University Press, 2010.
DRG's started the movement to the paperwork world. In 1992, came the PPO's:
A definition from Wikipedia,
In health insurance in the United States, a preferred provider organization (PPO), sometimes referred to as a participating provider organization or preferred provider option, is a managed care organization of medical doctors, hospitals, and other health care providers who have agreed with an insurer or a third-party administrator to provide health care at reduced rates to the top insurer's or administrator's clients.
During the time leading to 1992, doctors and hospitials were scrambling to form alliances. Again several layers of administration were added to deal with the complexity. of these relationships.
In the Wikipedia article, it is noted that the first PPO started in St. Luke's Medical Center (now Presbytarian/St. Luke's) in 1990.
Then there was this: from the Orlando Sentinel Jan 1, 1992:
The most far-ranging change in Medicare since it began setting hospital rates in 1983 takes effect today. This time, Medicare is setting rates for doctors.
And also this: in the 80's, the merging of hospitals created such behemoths as Humana, HealthOne, United Healthcare, etc. The more complex the organization, the more administrators needed..
These factors and others became out of control in the early 1990s and it became "Katie bar the door".
Please Log in or Create an account to join the conversation.
- Pony Soldier
-
- User is blocked
-

Less
More
- Posts: 4749
- Thank you received: 43
12 Mar 2021 07:52 #7
by Pony Soldier
Replied by Pony Soldier on topic THE PROBLEM OF HEALTH CARE IN ONE GRAPH
So it was when government became involved in healthcare to a much greater degree. Now it all makes sense....
Please Log in or Create an account to join the conversation.
- homeagain
-

- Mountain Legend
-

Less
More
- Posts: 12795
- Thank you received: 173
12 Mar 2021 07:59 #8
by homeagain
Replied by homeagain on topic THE PROBLEM OF HEALTH CARE IN ONE GRAPH
BINGO.....
Please Log in or Create an account to join the conversation.
- FredHayek
-
- Mountain Legend
-

Less
More
- Posts: 30759
- Thank you received: 179
12 Mar 2021 08:18 #9
by FredHayek
Thomas Sowell: There are no solutions, just trade-offs.
Replied by FredHayek on topic THE PROBLEM OF HEALTH CARE IN ONE GRAPH
Our GP's then got so tired of the paperwork and dealing with insurance companies that they sold out to a PPP organization.
At first it was fine, but then they found out they were employees and had to worry about productivity levels so patients got less time, you started to feeling rushed during your appointments. Now we are in an HMO, and not only do we rarely see the doctor any more, even some e-mails to her are intercepted and handled by underlings. It gets a little frustrating. And this has only become worse since Covid-19.
At first it was fine, but then they found out they were employees and had to worry about productivity levels so patients got less time, you started to feeling rushed during your appointments. Now we are in an HMO, and not only do we rarely see the doctor any more, even some e-mails to her are intercepted and handled by underlings. It gets a little frustrating. And this has only become worse since Covid-19.
Thomas Sowell: There are no solutions, just trade-offs.
Please Log in or Create an account to join the conversation.
- Pony Soldier
-
- User is blocked
-

Less
More
- Posts: 4749
- Thank you received: 43
12 Mar 2021 08:23 #10
by Pony Soldier
Replied by Pony Soldier on topic THE PROBLEM OF HEALTH CARE IN ONE GRAPH
I’ve never really needed healthcare up until about a decade ago so didn’t pay much attention. Since then, I’ve spent a fortune literally. The system is screwed and government needs to get out. I’ve spent in the high 6 figures over the last decade because things weren’t covered due to government regs.
Please Log in or Create an account to join the conversation.
Time to create page: 0.154 seconds