- Posts: 15746
- Thank you received: 320
COVID-19 Corona Virus - How You Can Prepare
- ScienceChic
-
 Topic Author
Topic Author
- Mountain Champion
-

By Rob Stein and Laurel Wamsley, NPR | February 25, 2020
CDC Corona Virus Disease 2019 Resource PageFederal health officials issued a blunt message Tuesday: Americans need to start preparing now for the possibility that more aggressive, disruptive measures might be needed to stop the spread of the new coronavirus in the U.S.
"It's not so much a question of if this will happen anymore, but more really a question of when it will happen — and how many people in this country will have severe illness," Dr. Nancy Messonnier of the Centers for Disease Control and Prevention told reporters during a briefing.
"We are asking the American public to work with us to prepare with the expectation that this could be bad," Messonnier said.
Those measures could include school closings, workplace shutdowns and canceling large gatherings and public events, she warned.
She stressed that the current risk remains low.
CDC / MMWR - "Update: Public Health Response to the Coronavirus Disease 2019 Outbreak — United States, February 24, 2020
Past Time to Tell the Public: “It Will Probably Go Pandemic, and We Should All Prepare Now”
by Jody Lanard and Peter M. Sandman | February 23, 2020
We are starting to hear from experts and officials who now believe a COVID-19 pandemic is more and more likely. They want to use the “P word,” and also start talking more about what communities and individuals can and should do to prepare. On February 22, Australian virologist Ian Mackay asked us for our thoughts on this phase of COVID-19 risk communication.
Here is our response.
Yes, it is past time to say “pandemic” – and to stop saying “stop”
Even officials who say very alarming things about the prospects of a pandemic mostly focus on how their agencies are preparing, not on how the people they misperceive as “audience” should prepare. “Audience” is the wrong frame. We are all stakeholders, and we don’t just want to hear what officials are doing. We want to hear what we can do too.
We want – and need – to hear advice like this:
- Try to get a few extra months’ worth of prescription meds, if possible.
- Think through now how we will take care of sick family members while trying not to get infected.
- Cross-train key staff at work so one person’s absence won’t derail our organization’s ability to function.
- Practice touching our faces less. So how about a face-counter app like the step-counters so many of us use?
- Replace handshakes with elbow-bumps (the “Ebola handshake”).
- Start building harm-reduction habits like pushing elevator buttons with a knuckle instead of a fingertip.
"Now, more than ever, the illusions of division threaten our very existence. We all know the truth: more connects us than separates us. But in times of crisis the wise build bridges, while the foolish build barriers. We must find a way to look after one another as if we were one single tribe.” -King T'Challa, Black Panther
The truth is incontrovertible. Malice may attack it. ignorance may deride it, but in the end, there it is. ~Winston Churchill
Please Log in or Create an account to join the conversation.
- homeagain
-

- Mountain Legend
-

- Posts: 12818
- Thank you received: 173
Please Log in or Create an account to join the conversation.
- ScienceChic
-
 Topic Author
Topic Author
- Mountain Champion
-

- Posts: 15746
- Thank you received: 320
Public Health - Seattle & King County @KCPubHealth 21m
To increase your chances of staying healthy, avoid crowded settings if possible, especially if you are over 60, or have other chronic health conditions such as diabetes, heart disease, lung disease, or a weakened immune system.
Do not go to the emergency room unless essential. Emergency rooms need to be able to serve those with the most critical needs. If you have symptoms like cough, fever, or other respiratory problems, contact your regular doctor first.
Johns Hopskins live tracking of COVID-19 Cases
World Health Organization Rolling Updates on Coronavirus Disease COVID-19
Pandemic Preparation from Ready.gov
During a Pandemic
Limit the Spread of Germs and Prevent Infection
- Avoid close contact with people who are sick.
- When you are sick, keep your distance from others to protect them from getting sick too.
- Cover your mouth and nose with a tissue when coughing or sneezing. It may prevent those around you from getting sick.
- Washing your hands often will help protect you from germs.
- Avoid touching your eyes, nose or mouth.
- Practice other good health habits. Get plenty of sleep, be physically active, manage your stress, drink plenty of fluids, and eat nutritious food.
Centers for Disease Control, February 29, 2020
Government of Canada Coronavirus disease (COVID-19): Outbreak updateOutbreaks of novel virus infections among people are always of public health concern. The risk from these outbreaks depends on characteristics of the virus, including how well it spreads between people, the severity of resulting illness, and the medical or other measures available to control the impact of the virus (for example, vaccine or treatment medications). The fact that this disease has caused illness, including illness resulting in death, and sustained person-to-person spread is concerning. These factors meet two of the criteria of a pandemic. As community spread is detected in more and more countries, the world moves closer toward meeting the third criteria, worldwide spread of the new virus.
While there is still much to learn about the unfolding situations in California, Oregon and Washington, preliminary information raises the level of concern about the immediate threat for COVID-19 for certain communities in the United States. The potential public health threat posed by COVID-19 is very high, to the United States and globally.
At this time, however, most people in the United States will have little immediate risk of exposure to this virus. This virus is NOT currently spreading widely in the United States. However, it is important to note that current global circumstances suggest it is likely that this virus will cause a pandemic. This is a rapidly evolving situation and the risk assessment will be updated as needed.
Current risk assessment:
- For the general American public, who are unlikely to be exposed to this virus at this time, the immediate health risk from COVID-19 is considered low.
- People in communities where ongoing community spread with the virus that causes COVID-19 has been reported are at elevated though still relatively low risk of exposure.
- Healthcare workers caring for patients with COVID-19 are at elevated risk of exposure.
- Close contacts of persons with COVID-19 also are at elevated risk of exposure.
- Travelers returning from affected international locations where community spread is occurring also are at elevated risk of exposure.
CDC has developed guidance to help in the risk assessment and management of people with potential exposures to COVID-19.
What May Happen
More cases of COVID-19 are likely to be identified in the coming days, including more cases in the United States. It’s also likely that person-to-person spread will continue to occur, including in communities in the United States. It’s likely that at some point, widespread transmission of COVID-19 in the United States will occur.
Widespread transmission of COVID-19 would translate into large numbers of people needing medical care at the same time. Schools, childcare centers, workplaces, and other places for mass gatherings may experience more absenteeism. Public health and healthcare systems may become overloaded, with elevated rates of hospitalizations and deaths. Other critical infrastructure, such as law enforcement, emergency medical services, and transportation industry may also be affected. Health care providers and hospitals may be overwhelmed. At this time, there is no vaccine to protect against COVID-19 and no medications approved to treat it. Nonpharmaceutical interventions would be the most important response strategy.
Research Papers Published About COVID-19
Search term COVID 19 at Pubmed.gov,
US National Library of Medicine National Institutes of Health
"Now, more than ever, the illusions of division threaten our very existence. We all know the truth: more connects us than separates us. But in times of crisis the wise build bridges, while the foolish build barriers. We must find a way to look after one another as if we were one single tribe.” -King T'Challa, Black Panther
The truth is incontrovertible. Malice may attack it. ignorance may deride it, but in the end, there it is. ~Winston Churchill
Please Log in or Create an account to join the conversation.
- ScienceChic
-
 Topic Author
Topic Author
- Mountain Champion
-

- Posts: 15746
- Thank you received: 320
Anthony S. Fauci, M.D., H. Clifford Lane, M.D., and Robert R. Redfield, M.D.
Author Affiliations
From the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD (A.S.F., H.C.L.); and the Centers for Disease Control and Prevention, Atlanta (R.R.R.).
The New England Journal of Medicine
February 28, 2020
DOI: 10.1056/NEJMe2002387
In their Journal article, Li and colleagues3 provide a detailed clinical and epidemiologic description of the first 425 cases reported in the epicenter of the outbreak: the city of Wuhan in Hubei province, China. Although this information is critical in informing the appropriate response to this outbreak, as the authors point out, the study faces the limitation associated with reporting in real time the evolution of an emerging pathogen in its earliest stages. Nonetheless, a degree of clarity is emerging from this report.
On the basis of a case definition requiring a diagnosis of pneumonia, the currently reported case fatality rate is approximately 2%.4 In another article in the Journal, Guan et al.5 report mortality of 1.4% among 1099 patients with laboratory-confirmed Covid-19; these patients had a wide spectrum of disease severity. If one assumes that the number of asymptomatic or minimally symptomatic cases is several times as high as the number of reported cases, the case fatality rate may be considerably less than 1%. This suggests that the overall clinical consequences of Covid-19 may ultimately be more akin to those of a severe seasonal influenza (which has a case fatality rate of approximately 0.1%) or a pandemic influenza (similar to those in 1957 and 1968) rather than a disease similar to SARS or MERS, which have had case fatality rates of 9 to 10% and 36%, respectively.2
The efficiency of transmission for any respiratory virus has important implications for containment and mitigation strategies. The current study indicates an estimated basic reproduction number (R0) of 2.2, which means that, on average, each infected person spreads the infection to an additional two persons. As the authors note, until this number falls below 1.0, it is likely that the outbreak will continue to spread. Recent reports of high titers of virus in the oropharynx early in the course of disease arouse concern about increased infectivity during the period of minimal symptoms.6,7
"Now, more than ever, the illusions of division threaten our very existence. We all know the truth: more connects us than separates us. But in times of crisis the wise build bridges, while the foolish build barriers. We must find a way to look after one another as if we were one single tribe.” -King T'Challa, Black Panther
The truth is incontrovertible. Malice may attack it. ignorance may deride it, but in the end, there it is. ~Winston Churchill
Please Log in or Create an account to join the conversation.
- ScienceChic
-
 Topic Author
Topic Author
- Mountain Champion
-

- Posts: 15746
- Thank you received: 320
For Immediate Release:
February 27, 2020
Statement From:
Commissioner of Food and Drugs - Food and Drug Administration
Stephen M. Hahn M.D.
As I have previously communicated, the FDA has been closely monitoring the supply chain with the expectation that the COVID-19 outbreak would likely impact the medical product supply chain, including potential disruptions to supply or shortages of critical medical products in the U.S.
A manufacturer has alerted us to a shortage of a human drug that was recently added to the drug shortages list. The manufacturer just notified us that this shortage is related to a site affected by coronavirus. The shortage is due to an issue with manufacturing of an active pharmaceutical ingredient used in the drug. It is important to note that there are other alternatives that can be used by patients. We are working with the manufacturer as well as other manufacturers to mitigate the shortage. We will do everything possible to mitigate the shortage.
Additional Information on Human Drugs
Since January 24, the FDA has been in touch with more than 180 manufacturers of human drugs, not only to remind them of applicable legal requirements for notifying the FDA of any anticipated supply disruptions, but also asking them to evaluate their entire supply chain, including active pharmaceutical ingredients (the main ingredient in the drug and part that produces the intended effects, e.g., acetaminophen) and other components manufactured in China.
Also, as part of our efforts, the FDA has identified about 20 other drugs, which solely source their active pharmaceutical ingredients or finished drug products from China. We have been in contact with those firms to assess whether they face any drug shortage risks due to the outbreak. None of these firms have reported any shortage to date. Also, these drugs are considered non-critical drugs.
We will remain in contact with manufacturers so that we can continue to assist them with any potential issues in the fastest way.
Medical Devices
We are aware of 63 manufacturers which represent 72 facilities in China that produce essential medical devices; we have contacted all of them. Essential devices are those that may be prone to potential shortage if there is a supply disruption. We are aware that several of these facilities in China are adversely affected by COVID-19, citing workforce challenges, including the necessary quarantine of workers. While the FDA continues to assess whether manufacturing disruptions will affect overall market availability of these products, there are currently no reported shortages for these types of medical devices within the U.S. market.
Regarding personal protective equipment—surgical gowns, gloves, masks, respirator protective devices, or other medical equipment designed to protect the wearer from injury or the spread of infection or illness—the FDA has heard reports of increased market demand and supply challenges for some of these products. However, the FDA is currently not aware of specific widespread shortages of medical devices, but we are aware of reports from CDC and other U.S. partners of increased ordering of a range of human medical products through distributors as some healthcare facilities in the U.S. are preparing for potential needs if the outbreak becomes severe.
It is important to note that no law exists requiring medical device manufacturers to notify the FDA when they become aware of a circumstance, including discontinuation of a product, that could lead to a potential shortage, and manufacturers are not required to respond when the FDA requests information about potential supply chain disruption. As with prior emergencies, the FDA has taken proactive steps to establish and remain in contact with medical device manufacturers and others in the supply chain, including hospitals and group purchasing organizations. The agency also encourages manufacturers and healthcare facilities to report any supply disruptions to the device shortages mailbox, This email address is being protected from spambots. You need JavaScript enabled to view it.. This mailbox is closely monitored and has proven to be a valuable surveillance resource to augment FDA efforts to detect and mitigate potential supply chain disruption.
Biologics and Blood Supply
The FDA is not aware of any cellular or gene therapies that are made in China for the U.S. market. There are no shortages of biologics to report at this time.
The potential for transmission of COVID-19 by blood and blood components is unknown at this time; however, respiratory viruses, in general, are not known to be transmitted by blood transfusion. Further, there have been no reported cases of transfusion-transmitted COVID-19.
The FDA has made information available to blood establishments and to establishments that manufacture human cells, tissues, or cellular or tissue-based products that may wish to consider additional donor screening measures in response to the COVID-19 outbreak.
Food
We are not aware of any reports at this time of human illnesses that suggest COVID-19 can be transmitted by food or food packaging. However, it is always important to follow good hygiene practices (i.e., wash hands and surfaces often, separate raw meat from other foods, cook to the right temperature, and refrigerate foods promptly) when handling or preparing foods.
Animal Drugs
There are 32 animal drug firms that make finished drugs or source active pharmaceutical ingredients in China for the U.S. The FDA has contacted all 32 firms and no shortages have been reported at this time. However, six of those firms have indicated that they are seeing disruptions in the supply chain that soon could lead to shortages. The FDA is working with these firms to help identify interventions to mitigate potential shortages.
Additional Resources
The FDA is using all our existing authorities to address COVID-19, and we welcome the opportunity to work with Congress to further strengthen our response capabilities and emergency preparedness. There are four specific proposals included in the President’s budget that would better equip the FDA to prevent or mitigate medical product shortages.
- Lengthen Expiration Dates to Mitigate Critical Human Drug Shortages: Shortages of certain critical drugs can be exacerbated when drugs must be discarded because they exceed a labeled shelf-life due to unnecessarily short expiration dates. By expanding the FDA’s authority to require, when likely to help prevent or mitigate a shortage, that an applicant evaluate, submit studies to the FDA, and label a product with the longest possible expiration date that the FDA agrees is scientifically justified, there could be more supply available to alleviate the drug shortage or the severity of a shortage.
- Improve Critical Infrastructure by Requiring Risk Management Plans: Enabling the FDA to require application holders of certain drugs to conduct periodic risk assessments to identify the vulnerabilities in their manufacturing supply chain (inclusive of contract manufacturing facilities), and develop plans to mitigate the risks associated with the identified vulnerabilities would enable the FDA to strengthen the supply chain by integrating contingencies for emergency situations. Currently, many medical product manufacturers lack plans to assess and address vulnerabilities in their manufacturing supply chain, putting them, and American patients, at risk for drug supply disruptions following disasters (e.g., hurricanes) or in other circumstances.
- Improve Critical Infrastructure through Improved Data Sharing and Require More Accurate Supply Chain Information: Empowering the FDA to require information to assess critical infrastructure, as well as manufacturing quality and capacity, would facilitate more accurate and timely supply chain monitoring and improve our ability to recognize shortage signals.
- Establish Reporting Requirements for Device Manufacturers: The FDA does not have the same authorities for medical device shortages as it does for drugs and biological products. For instance, medical device manufacturers are not required to notify the FDA when they become aware of a circumstance that could lead to a device shortage or meaningful disruption in the supply of that device in the U.S., nor are they required to respond to inquiries from the FDA about the availability of devices. Enabling the FDA to have timely and accurate information about likely or confirmed national shortages of essential devices would allow the agency to take steps to promote the continued availability of devices of public health importance. Among other things, the FDA proposes to require that firms notify the agency of an anticipated meaningful interruption in the supply of an essential device; require all manufacturers of devices determined to be essential to periodically provide the FDA with information about the manufacturing capacity of the essential devices they manufacture; and authorize the temporary importation of devices where the benefits of the device in mitigating a shortage outweigh the risks presented by the device that could otherwise result in denial of importation of the device into the U.S.
We also continue to aggressively monitor the market for any firms marketing products with fraudulent COVID-19 diagnosis, prevention or treatment claims. The FDA can and will use every authority at our disposal to protect consumers from bad actors who take advantage of a crisis to deceive the public, including pursuing warning letters, seizures or injunctions against products on the market that are not in compliance with the law, or against firms or individuals who violate the law.
We know the public may have questions or concerns for the FDA as a result of this outbreak, including you and your family’s risk of exposure, or whether your critical medical products are safe and will continue to be available in the future. The FDA is working around the clock to monitor and mitigate emerging coronavirus issues through collaborative efforts with federal partners, international regulators and medical product developers and manufacturers to help advance response efforts to combat the COVID-19 outbreak.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
###
"Now, more than ever, the illusions of division threaten our very existence. We all know the truth: more connects us than separates us. But in times of crisis the wise build bridges, while the foolish build barriers. We must find a way to look after one another as if we were one single tribe.” -King T'Challa, Black Panther
The truth is incontrovertible. Malice may attack it. ignorance may deride it, but in the end, there it is. ~Winston Churchill
Please Log in or Create an account to join the conversation.
- homeagain
-

- Mountain Legend
-

- Posts: 12818
- Thank you received: 173
THERE ARE NOW TWO STRAINS,recent testing indicates,one is stronger and one weaker, it appears it has mutated OR we are just now understanding the composition.
Please Log in or Create an account to join the conversation.
- ScienceChic
-
 Topic Author
Topic Author
- Mountain Champion
-

- Posts: 15746
- Thank you received: 320
CDC Mitigation Slides
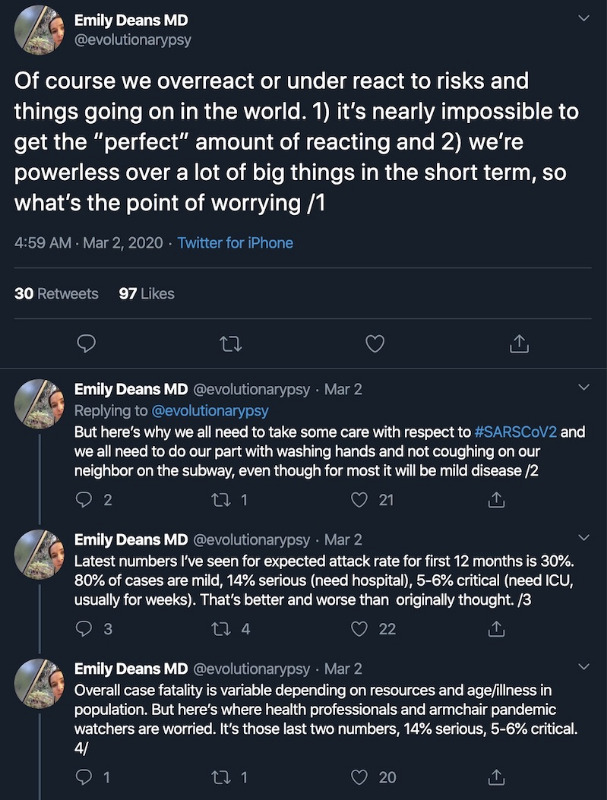
Good thread from Emily Deans MD
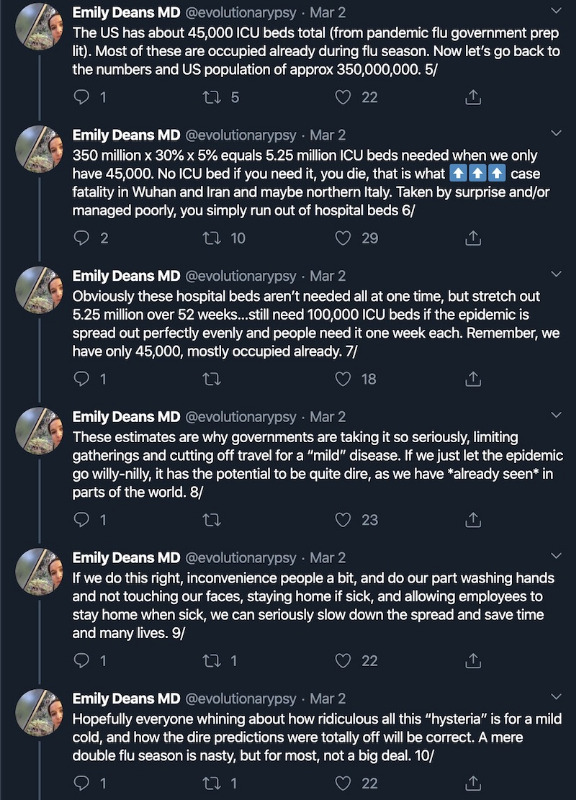
The CDC has now changed testing requirements:
"Now, more than ever, the illusions of division threaten our very existence. We all know the truth: more connects us than separates us. But in times of crisis the wise build bridges, while the foolish build barriers. We must find a way to look after one another as if we were one single tribe.” -King T'Challa, Black Panther
The truth is incontrovertible. Malice may attack it. ignorance may deride it, but in the end, there it is. ~Winston Churchill
Please Log in or Create an account to join the conversation.
- ScienceChic
-
 Topic Author
Topic Author
- Mountain Champion
-

- Posts: 15746
- Thank you received: 320
More at www.cdc.gov/coronavirus/2019-ncov/specif...siness-response.htmlRecommended strategies for employers to use now:
Additional Measures in Response to Currently Occurring Sporadic Importations of the COVID-19:
- Actively encourage sick employees to stay home
- Separate sick employees
- Emphasize staying home when sick, respiratory etiquette and hand hygiene by all employees
- Perform routine environmental cleaning
- Advise employees before traveling to take certain steps
- Employees who are well but who have a sick family member at home with COVID-19 should notify their supervisor and refer to CDC guidance for how to conduct a risk assessment of their potential exposure.
- If an employee is confirmed to have COVID-19, employers should inform fellow employees of their possible exposure to COVID-19 in the workplace but maintain confidentiality as required by the Americans with Disabilities Act (ADA). Employees exposed to a co-worker with confirmed COVID-19 should refer to CDC guidance for how to conduct a risk assessment of their potential exposure.
Park County Public Health Coronavirus COVID-19 Documentation
Jeffco Public Health Department Coronavirus 2019 - COVID-19
There is an expanding global outbreak of respiratory illness caused by a novel (new) coronavirus, named COVID-19. JCPH is closely monitoring this outbreak in collaboration with other national, state and local partners. This is a rapidly evolving situation. You can find the most recent data on confirmed cases and other information here.
If you have symptoms and think you have been exposed, call a health care provider. Please call ahead before you go.
For general questions about COVID-19, call CO-HELP at 303-389-1687 or 1-877-462-2911, or email This email address is being protected from spambots. You need JavaScript enabled to view it. for answers in English and Spanish.
From Jefferson County:
Want to learn about Coronavirus (COVID-19) and what Jefferson County is doing to be prepared? Check out the Q&A with the Lakewood Sentinel.
How has Jeffco prepared for a major outbreak?
Even though there have been no cases of COVID-19 in Jefferson County or Colorado, and though the immediate risk to most people is low, Jefferson County Public Health, the Colorado Department of Public Health and Environment (CDPHE) and our health and medical partners are prepared. Jefferson County Public Health has conducted all-hazards planning for nearly two decades, and we are highly trained to respond to emerging threats just like this.
Since the start of the outbreak, we have been taking a proactive approach working closely with CDC, CDPHE and other partners to:
• Provide timely information about the outbreak to our community.
• Share guidance with health care providers so they know how to safely care for people with possible COVID-19 infection.
• Support local hospitals and other health and medical partners with requests for information and logistics.
• Actively monitor the situation and refine our response and recovery plans.
We have also activated our Jefferson County Public Health Emergency Operations Plan and are using the incident command system to allow for enhanced and coordinated response efforts. Basically, this allows us to secure the resources we need and utilize the full breadth of subject matter expertise that we have across our workforce to prepare. This structure also allows us to align efforts with other response partners.
lakewoodsentinel.com/stories/qampa-with-...e-coronavirus,294875
"Now, more than ever, the illusions of division threaten our very existence. We all know the truth: more connects us than separates us. But in times of crisis the wise build bridges, while the foolish build barriers. We must find a way to look after one another as if we were one single tribe.” -King T'Challa, Black Panther
The truth is incontrovertible. Malice may attack it. ignorance may deride it, but in the end, there it is. ~Winston Churchill
Please Log in or Create an account to join the conversation.
- ScienceChic
-
 Topic Author
Topic Author
- Mountain Champion
-

- Posts: 15746
- Thank you received: 320
Sawyer D'Argonne, Summit Daily News This email address is being protected from spambots. You need JavaScript enabled to view it. | March 4, 2020
FRISCO — A patient at St. Anthony Summit Medical Center in Frisco is being tested for coronavirus, according to a representative with the hospital.
The patient, who has a recent history of travel to Italy, came into the hospital’s emergency department Wednesday afternoon with a possible respiratory illness, according to a statement from hospital spokesman Brent Boyer. The hospital is investigating the possible case of novel coronavirus in collaboration with the Colorado Department of Public Health and Environment. Results of a test from the Centers for Disease Control and Prevention are expected back within 24 hours.
"Now, more than ever, the illusions of division threaten our very existence. We all know the truth: more connects us than separates us. But in times of crisis the wise build bridges, while the foolish build barriers. We must find a way to look after one another as if we were one single tribe.” -King T'Challa, Black Panther
The truth is incontrovertible. Malice may attack it. ignorance may deride it, but in the end, there it is. ~Winston Churchill
Please Log in or Create an account to join the conversation.
- ScienceChic
-
 Topic Author
Topic Author
- Mountain Champion
-

- Posts: 15746
- Thank you received: 320
Staff report, This email address is being protected from spambots. You need JavaScript enabled to view it. | March 2, 2020
The state laboratory at the Colorado Department of Public Health and Environment is now equipped to test for cases of coronavirus, according to state officials.
Before now, testing for COVID-19 had been conducted only by the Centers for Disease Control and Prevention. With new capacities for testing at the state level, officials are hoping to be more nimble in responding to and controlling the disease if it is found in Colorado.
For more information, resident’s can reach out to Colorado’s novel coronavirus hotline at 303-389-1687 or 1-877-462-2911. Residents also can reach out to This email address is being protected from spambots. You need JavaScript enabled to view it. or visit the state’s public health web page.
"Now, more than ever, the illusions of division threaten our very existence. We all know the truth: more connects us than separates us. But in times of crisis the wise build bridges, while the foolish build barriers. We must find a way to look after one another as if we were one single tribe.” -King T'Challa, Black Panther
The truth is incontrovertible. Malice may attack it. ignorance may deride it, but in the end, there it is. ~Winston Churchill
Please Log in or Create an account to join the conversation.